Blog
The 1918-20 influenza pandemic: A retrospective in the time of COVID-19
The influenza pandemic of 1918 (the Spanish Flu) is by far the greatest humanitarian disaster caused by an infectious disease in modern history. It infected over a quarter of the world’s population and killed over 50 million people. The brunt of the pandemic was borne by countries in the periphery (the present-day developing countries). Epidemiologists and health scientists often draw on this experience as the worst-case scenario when estimating pandemic mortality.
It's easy to see why parallels are drawn between the 1918 pandemic and the recent COVID-19 pandemic. And while reasoning by historical analogy does not provide definitive lessons, it does help to identify areas where more thinking and research is required for the design of evidence-based public policy interventions. The 1918 pandemic spawned a deep literature of scientific inquiry related to public health which provides several lessons for the post-COVID world. Our new Cambridge Elements publication provides a review of this literature, and covers many of these lessons in detail.
COVID-19 through the prism of 1918 pandemic
The 1918 pandemic and COVID-19 are caused by two unrelated respiratory viruses: the H1NI strain of avian influenza (Type A) and the severe acute respiratory syndrome coronavirus, SARS-COV-2, respectively. However, their transmission is similar. Both viruses have the inherent feature of a high mutation rate with the possibility of efficiently transmitting from person to person and mutating to become more virulent. In both cases, infected individuals can transmit the virus pre-symptomatically. Therefore, as public health crises, they are strikingly similar in their clinical, pathological, and epidemiological features, and in public health and medical responses.
The virus that caused the 1918 pandemic eventually turned out to be a foundation virus, descendants of which persist to this date. Whether the COVID-19 virus, SARS-COVID 2, will persist as a foundation virus or die out in the face of growing population immunity is bound to perplex medical science for years to come. If we’re drawing lessons from the 1918 pandemic, a key thing to note is that although the virus became a foundation virus, its time as a pandemic was short lived, and it became much less life-threatening as time passed.
We live in a time when the world is far more susceptible to unification by infectious disease than it was in the early 20th century. The speed and extent of the global spread of COVID-19 has been unparalleled in world history. However, COVID-19 also arrived at a time of remarkable medical advance: rapid viral diagnostics, diagnostic imaging, antibiotics, antivirals, intensive care units with ventilators with membrane oxygenation, and, most importantly, advances in virology that fostered rapid development of a vaccine.
Although the virus can spread across the world more easily, the mortality rate of COVID-19 is yet to reach the levels of the 1918 pandemic. The socioeconomic cost is likely to be determined rather by morbidity rates (the incidence of infection) rather than mortality rates (the number of people who die of the infection), and their related economic disruptions.
Figure 1: Mortality of the 1918–1920 influenza pandemic by world geographical regions (%)
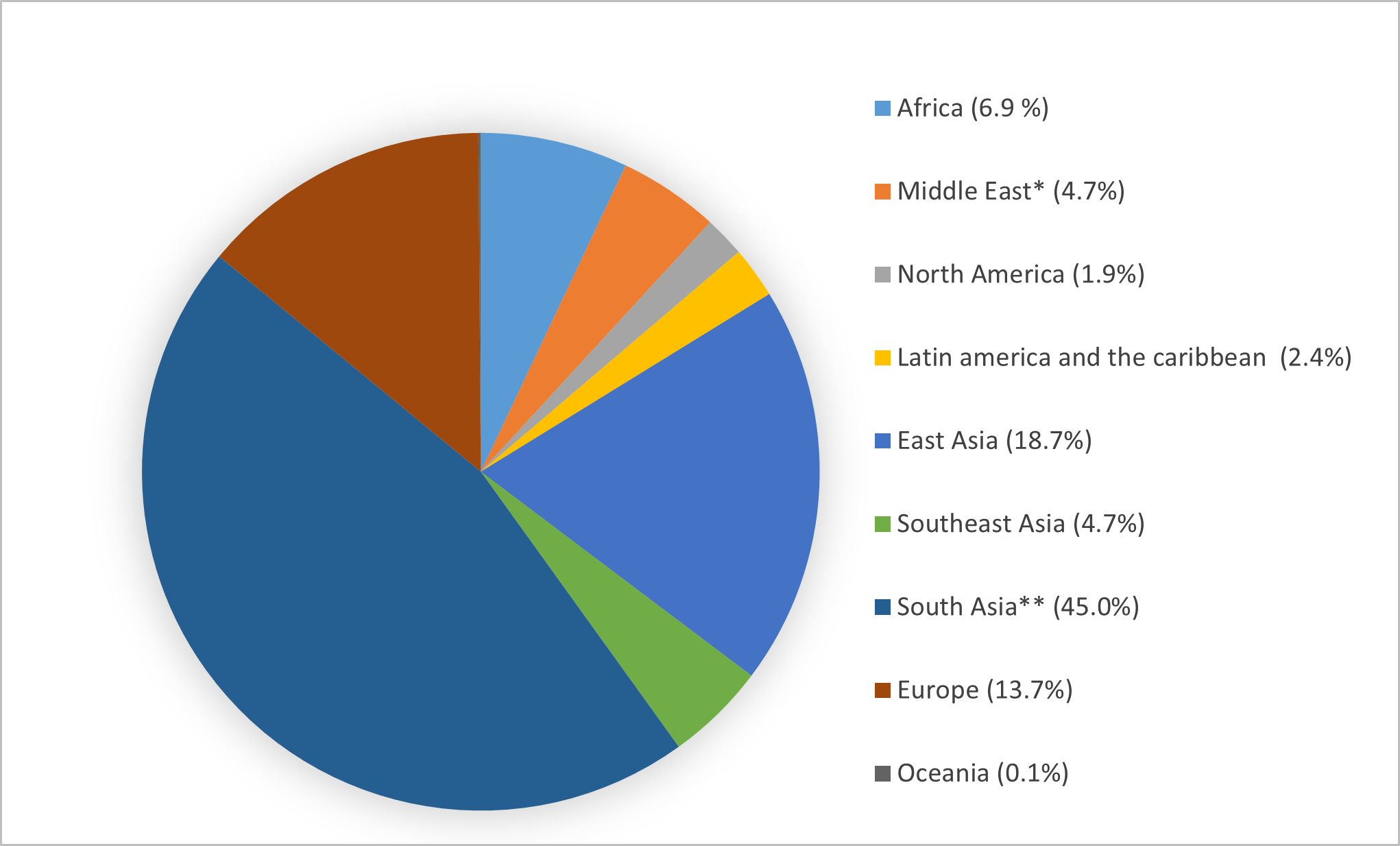
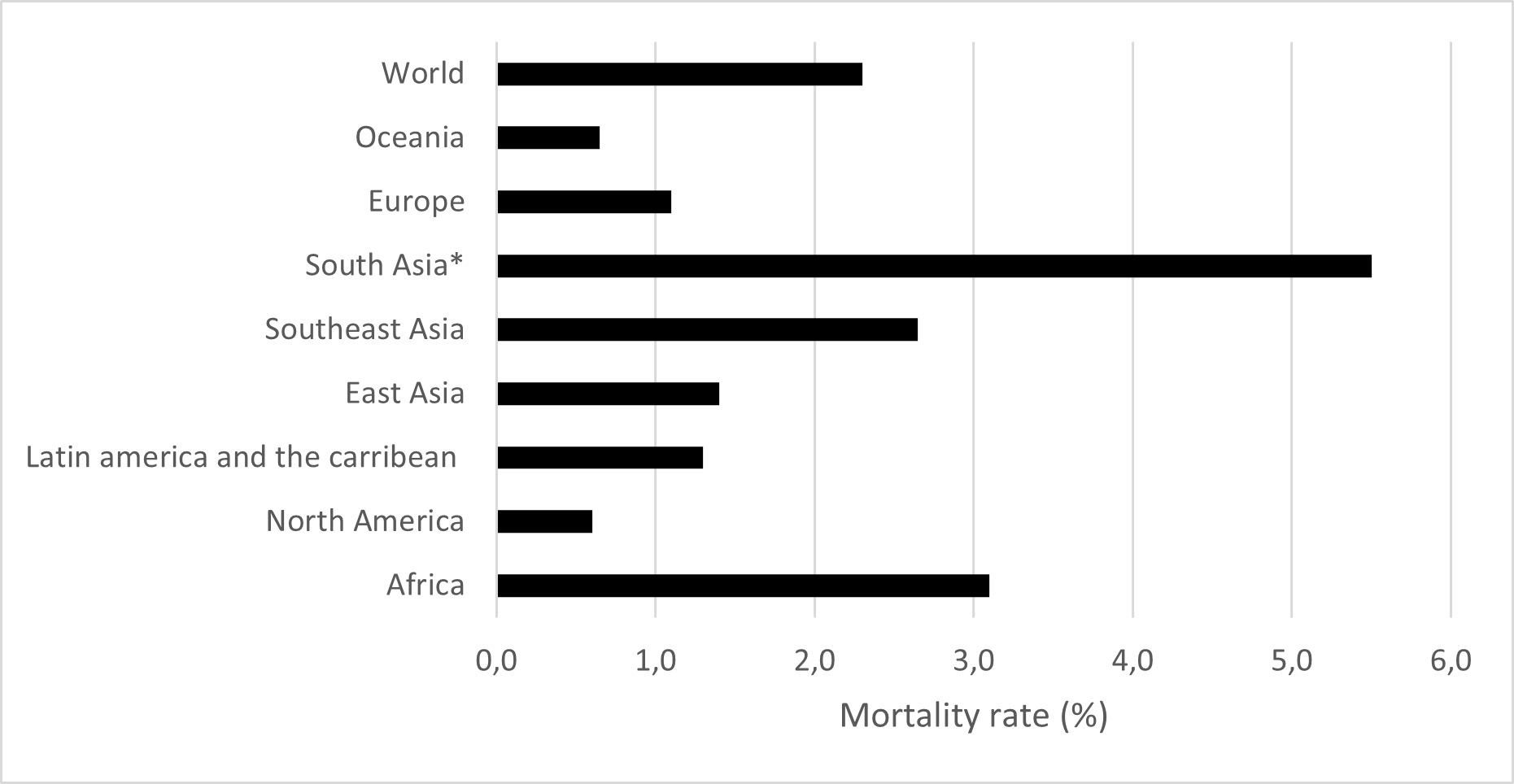
Figure 2: Mortality rates of the 1918–1920 influenza pandemic by world geographical regions (%)
Since the vast majority of infected people ultimately survive COVID-19, the impacts likely to dominate the post-pandemic research agenda will be on morbidity-related factors. More research about how COVID-19 impacts pregnant people and their babies, how it impacts people over time (e.g., long COVID), and how it interacts with other diseases to increase mortality risk is still needed. More needs to be known, too, about how these impacts have affected future levels of human capital around the world.
Reflecting on the lessons
Based on our recent review of the literature spawned by the 1918 pandemic, our new Cambridge Elements illustrates that perhaps the most important lesson of the 1918 pandemic relates to the unequal distribution of the burden between developed and developing economies. At a time when existing therapeutic intervention made little difference, intercountry differences in the death toll of the 1918 pandemic were strongly mediated by the state of economic advancement, with poverty and deprivation and associated comorbidity playing a bigger role than virulence itself.
The global experience vividly illustrated that mortality caused by a pandemic is a reflection of the socioeconomic and political order that the pathogen encounters. Whether advances in medical intervention will reduce the inequality of the distribution of COVID-19’s impacts remain to be seen.
Today, vaccines are the cornerstone of our fight against viral disease. The speedy development of effective COVID-19 vaccines within a year of the onset of the pandemic is a stellar achievement of modern viral research that was itself spawned by the 1918 pandemic. But the possibility of mutations, abrupt dissipation, and uncertainty of duration of the pandemic makes massive investments in vaccine development risky from a private enterprise perspective. This creates a hurdle on the path towards equitable vaccine distribution. If production is limited, so too is distribution. As we often see, it is those in the Global South who are left behind.
Governments and international development organizations have an important role to play to alleviate the commercial risk involved in the development and production of vaccines that pharmaceutical companies are hesitant to bear on their own. Great achievements in research and development, especially medical ones, usually require the support of public institutions.
Preparing for the next pandemic
COVID-19 could be considered the pandemic foretold. As we discuss in the new publication, there were ample signs and warnings about likelihood of a largescale pandemic event, based on the extensive scientific research on the 1918 pandemic done in recent decades. Although unprecedented in many ways, COVID-19 was not unpredictable.
Further, the nature of globalization has shown that going forward pandemic preparedness cannot be regarded as a local or national issue, as such pandemic planning and preparedness must be an integral part of the international development agenda. Also because of the damage that not being prepared has caused to the progress made towards the Sustainable Development Goals with poverty backsliding, access to education halted, not to mention the economic downturn, and more. To do this well, we will need to bring the ‘economics of infectious disease’ to the forefront of scientific research and the public policy debate.
The views expressed in this piece are those of the author(s), and do not necessarily reflect the views of the Institute or the United Nations University, nor the programme/project donors.
Prema-chandra Athukorala is Emeritus Professor of Economics, working in the Crawford School of Public Policy at The Australian National University is Asia, the Pacific’s leading graduate public policy school.
Chaturica Athukorala is based at the Department of Medical Imaging, Canberra Hospital, Australia.
 Join the network
Join the network









